Toward the end of most cancer surgeries comes a race against the clock, as the surgeon faces a high-stakes decision. Take out too much healthy tissue along with the tumor, and a patient could require longer to recover and experience a lower quality of life. Leave behind any cancerous cells, and the patient could need a second surgery and face an increased chance the tumor will regrow. “Tumors are sneaky,” said Alastair Thompson, a surgeon at Baylor College of Medicine who specializes in breast cancer. “They can have little threads of tumor cells that may be impossible to feel or see with the naked eye.” Determining whether the harmful tissue has been entirely excised requires a series of complicated procedures—all taking place within twenty to forty minutes, in order to minimize the risk of surgical complications to the anesthetized patient.
To enable this important call, the surgeon hands the tumor off to a pathologist, a physician whose specialty is understanding the effects of disease on the body’s tissues and fluids. What follows is an examination of the marginal layer of healthy cells that the surgeon removed along with the tumor in an attempt to ensure every last bit of cancer is gone. If those margin cells are noncancerous, then the surgeon removed enough tissue. If they show hallmarks of cancer—such as varied sizes and shapes or overly large nuclei—then the surgeon needs to remove more tissue.
The pathologist’s work requires highly specialized skills and training. It’s also difficult. An estimated one in four lumpectomies, which involve the removal of breast tissue, end without the full tumor excised. For other types of tumors, although the exact numbers vary according to the type of surgery, the rate at which cancer cells get left behind is significant.
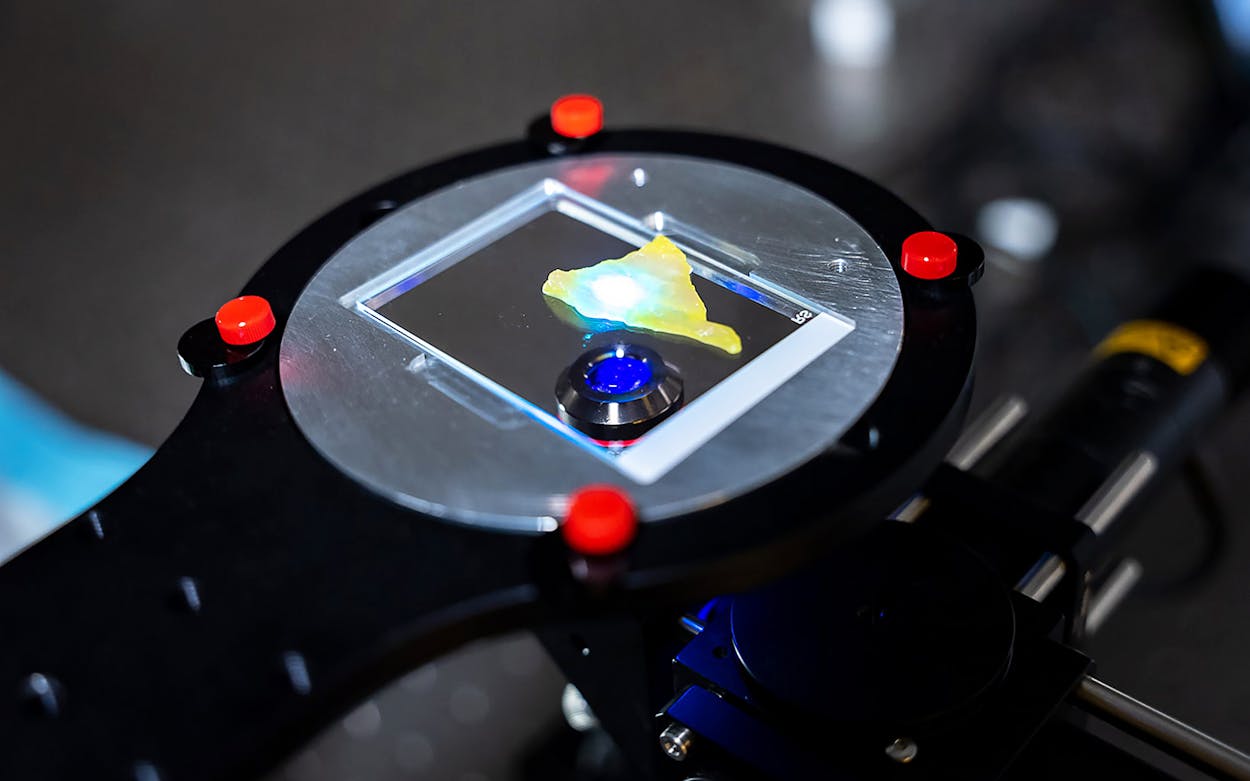
But a new microscope, developed by researchers at Rice University in Houston, has the potential to greatly simplify this analysis. The device, called a deep-learning extended depth-of-field microscope, or DeepDOF for short, combines a conventional fluorescent microscope with a special type of lens and software that enhances the images it captures. The prototype for this microscope was recently described in a paper in the journal Proceedings of the National Academies of Science.
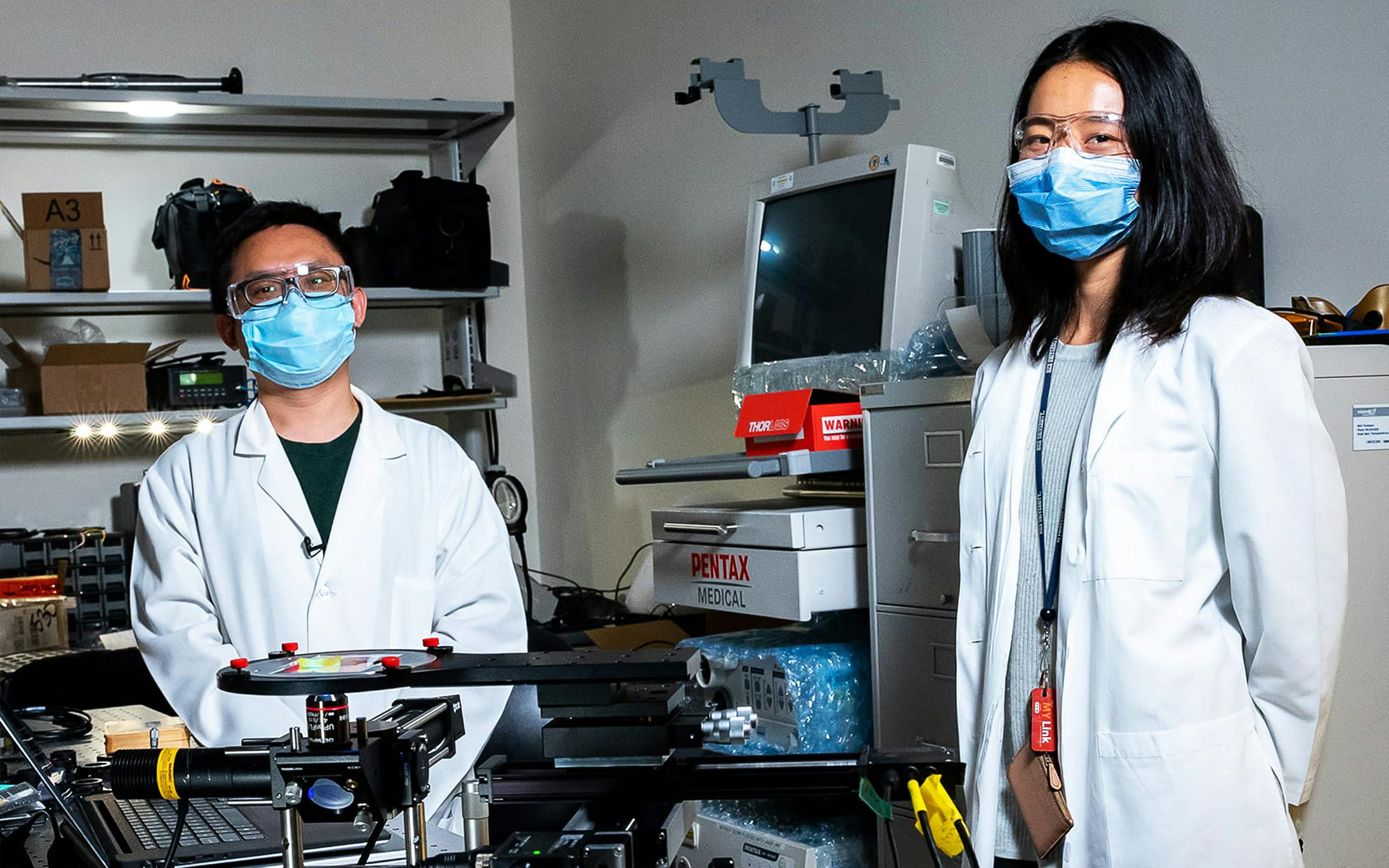
“This is a very cheap, very rapid way to get the same kind of information without having to have the infrastructure you would typically have in an academic medical center,” said Rebecca Richards-Kortum, a professor of biomedical engineering at Rice, and one of the lead researchers for the project.

During a typical oncological surgery, the pathologist first cuts the excised tumor into extremely thin slices, about three or four millimeters thick, and examines those by eye. Following this gross assessment, the slices have to go under a microscope, but to do that right, the sample must be even thinner and remain incredibly flat. The pathologist has to select a small piece of tissue, embed it in a thick gel-like substance, and flash-freeze the sample. Then a piece of equipment called a cryotome trims the sample down to just five thousandths of a millimeter thick. Finally the sample is treated with a dye that visibly outlines the structures of individual cells before it’s placed under the microscope.
As the pathologist works, precious minutes are ticking away with the surgeon and patient standing by. Each step of the process also introduces opportunities for errors. Some tissues, like those in the breast, don’t freeze well. Slices can easily wrinkle, and the embedding process can leave behind dark specks, resulting in a poor image. “If there are any challenges with getting a nice section or image, then that makes your life that much harder,” said Nicholas Reder, a pathologist and spokesperson for the College of American Pathologists.
There are often also significant concerns about losing too much of the sample along the way to make a determination, since each cut means discarding a little bit of the tissue. Especially for surgeries in sensitive areas, such as the neck or the brain, that sample tissue is precious. Even the tiniest loss can force a surgeon into an even more difficult decision between continuing the surgery or ending it without being completely sure every bit of cancer is gone. “The most common phrase uttered by a pathologist is ‘Could you send more tissue?’” Reder said.
Rice’s DeepDOF promises to eliminate the need to freeze the sample and to make those extremely thin slices via the cryotome. That’s because instead of a light microscope, which requires a sample thin enough to allow light to pass through, the DeepDOF uses a fluorescent microscope, which bounces light off the surface of the sample. Furthermore, to circumvent the need for a perfectly flat sample, the DeepDOF uses a phase mask, which allows it to capture an image of a bumpy surface. To address the drawback of this approach—a slightly blurred image—the DeepDOF’s software employs deep learning, a form of artificial intelligence that learns patterns after being fed large amounts of data. In this case, DeepDOF’s programming was exposed to matched blurred and high-resolution images for hundreds of tissue samples, as well as images of various types of cancer cells, to enable its recognition of both healthy and cancerous cells. Using this base of knowledge, DeepDOF “sharpens” the blurred image, creating the high-resolution image the pathologist needs in order to perform an analysis.
DeepDOF’s approach could well mean fewer repeat surgeries and healthier outcomes for patients. There is reduced risk of the sample being compromised by the process, as well as fewer chances for human error. The microscope could also help address inequities in health-care resources, since it works by modifying a widely available microscope via a low-cost addition. It reduces the expertise required to prepare tissue samples, allowing that to be handled by a trained technician who could send images elsewhere for analysis—helpful for a small hospital without a staff pathologist, or for a medium-sized hospital with an overburdened pathologist whose workload doesn’t allow for a quick analysis. And it could mean even more outside the United States, for nations with few trained pathologists.
“The U.S. has roughly one pathologist for every twenty thousand people,” Richards-Kortum said. “In a lot of African countries, there’s one pathologist for every five hundred thousand or one million people. Just having actual trained health-care providers is a huge obstacle.”
Addressing these inequities is a major hallmark of Richards-Kortum’s work, for which she received a MacArthur “genius grant” in 2015 and has also included developing low-cost machines for treating jaundice in newborns, as well as a breathing machine for premature babies.
The DeepDOF microscope must still be tested against a variety of tissue samples, to determine how well it will hold up in a clinical setting, but the potential is exciting to pathologists like Reder. “There’s still a relatively long road, but the need is there,” he said. “The technology used in pathology is fundamentally the same from the early 1900s. It’s barely changed over the past one hundred years.”
- More About:
- Health
- Rice University
- Cancer
- Houston