Now I’m going to percuss,” Frederick Wang says just before delivering a sharp tap to Mason Danna’s back. “Can you exhale and hold that exhale for me?”
With Wang clad in a white lab coat and Danna perched on an examination table in a hospital gown, the pair look like a doctor conducting a routine physical and his patient. Except that Wang nervously smirks and chuckles as he asks Danna to move various body parts about. And a third party, Ken Lavergne, is observing each step and scribbling notes.
Wang and Danna are, in fact, Texas A&M University medical students learning to conduct a head-to-toe examination of a patient. Lavergne, a teaching associate, is here, in this small room in Houston Methodist Hospital, to suggest improvements to their technique. When Wang is finished, the two young men will switch roles.
“No signs of scoliosis,” Wang says as he runs his hands along Danna’s back. “I’m going to palpate down the spine, on the side of the spine, transverse processes. Any tenderness? I’m going to find your sacroiliac joint.”
Anyone who isn’t a medical professional will probably need a translation of what Wang is saying. “Palpate” is doctor-speak for examining by touch. Transverse processes are the bony projections off the sides of each vertebra. Sacroiliac joints sit between your hip bones and your spine.
Medical school requires mastering a distinctive language, and Wang and Danna, who are only a few months into their training, will have to learn many more vocabulary words before they get their degrees. To become an MD in the United States, students typically spend two years in classrooms and labs, listening to lectures and memorizing vast reams of terminology regarding human anatomy, drugs, and diseases. That’s followed by two years of supervised clinical training, when they are drilled in medicine’s established best practices.
What’s not prioritized—what’s often actively discouraged—is thinking beyond medicine’s established vocabulary and methods. But as scientific advances have made the tools available to physicians exponentially more complex, some educators have begun to wonder whether medicine might be well served by a new sort of doctor—one schooled not merely in what the latest technology does but also in how it works. That sort of physician would be equipped not only to make better use of existing medical tools and methods but to envision ways to improve them.
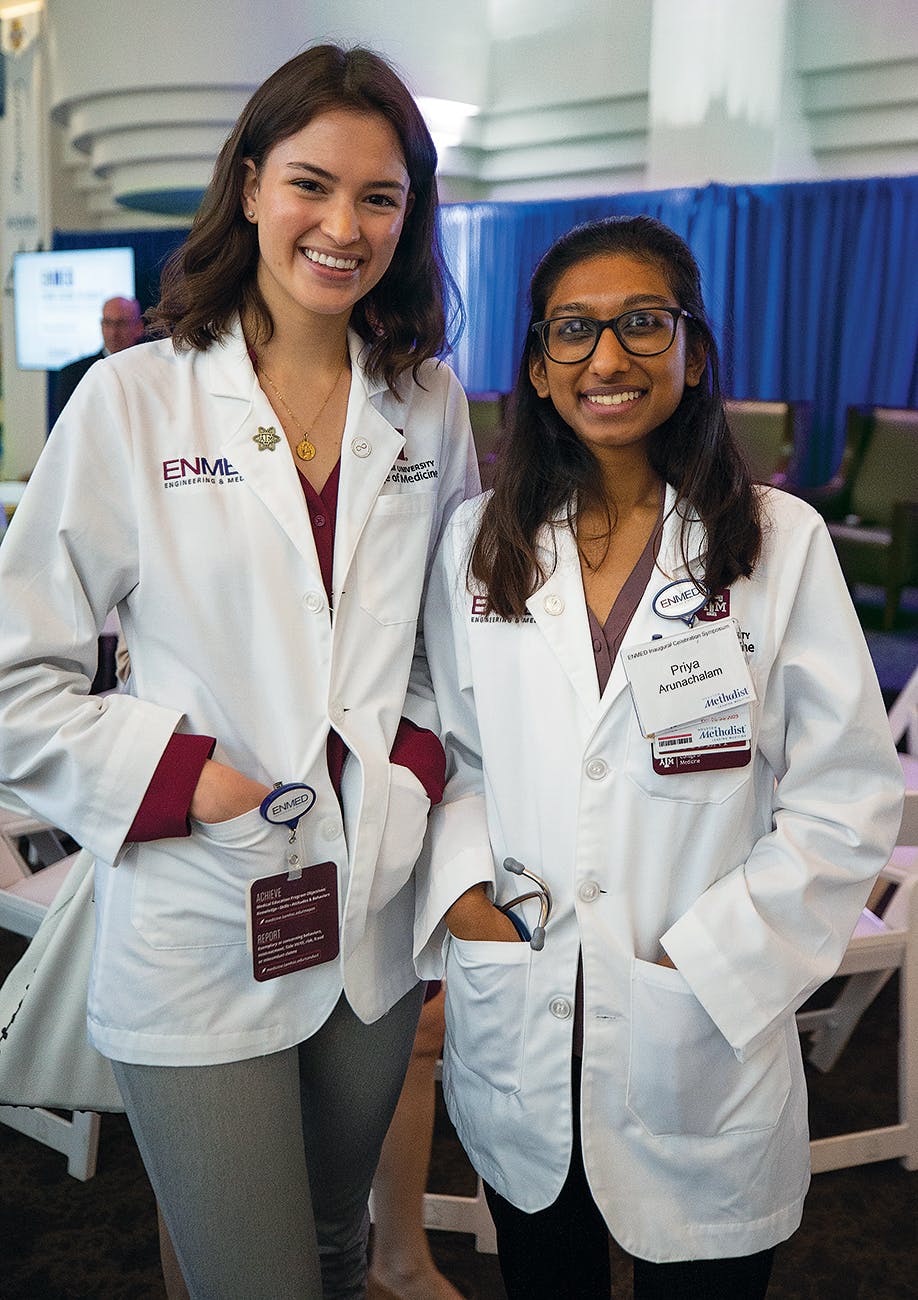
One result of this sort of thinking is the inaugural class of EnMed, an offshoot of Texas A&M’s medical program, that began this past June. The school has maintained a partnership with Houston Methodist since 2014, sending some of its students there each year to complete the clinical rotation portion of their educations. But this new venture is unlike virtually any other medical training program in the world.
Where most medical schools favor applicants with science degrees—biology and chemistry usually foremost among them—EnMed selects students, such as Wang and Danna, with a background in engineering or computer science. The expectation is that they will be able to apply their prior educations to their medical classes in unusual ways. “Take petroleum engineers,” says Dr. Timothy Boone, Houston Methodist’s head of urology, who also oversees the hospital’s academic partnerships. “It’s pumps and pipes and valves. So maybe they’re the new cardiovascular surgeons because they’re bringing the fluid dynamics side of engineering into cardiovascular surgery.”
This collaboration between Houston Methodist and A&M’s engineering and medical schools views its future graduates, who will earn both an MD and an engineering master’s degree, as more than just doctors. EnMed’s leadership calls them “physicianeers.”
In late November, two members of EnMed’s inaugural class, Pranav Gadangi and Evan George, showed me around the program’s temporary headquarters on the sixth floor of Houston Methodist’s West Pavilion building, on the sprawling Texas Medical Center campus. The student lounge and locker-lined hallway give the space the feel of a small high school.
Gadangi, who has a bachelor’s degree in biomedical engineering from Texas A&M, and George, a computer science graduate of the University of Texas at Dallas, seem typical of the first EnMed cohort. The class of 25 students is largely male (17 of the 25), and 21 of them are graduates of Texas universities (including 11 from A&M). The four other students come from top-notch schools—Johns Hopkins, Brown, Duke, and West Point—boasting degrees in chemical, petroleum, electrical, and nuclear engineering. EnMed expects to have 35 students in next year’s class and, eventually, an enrollment of 50 each year.
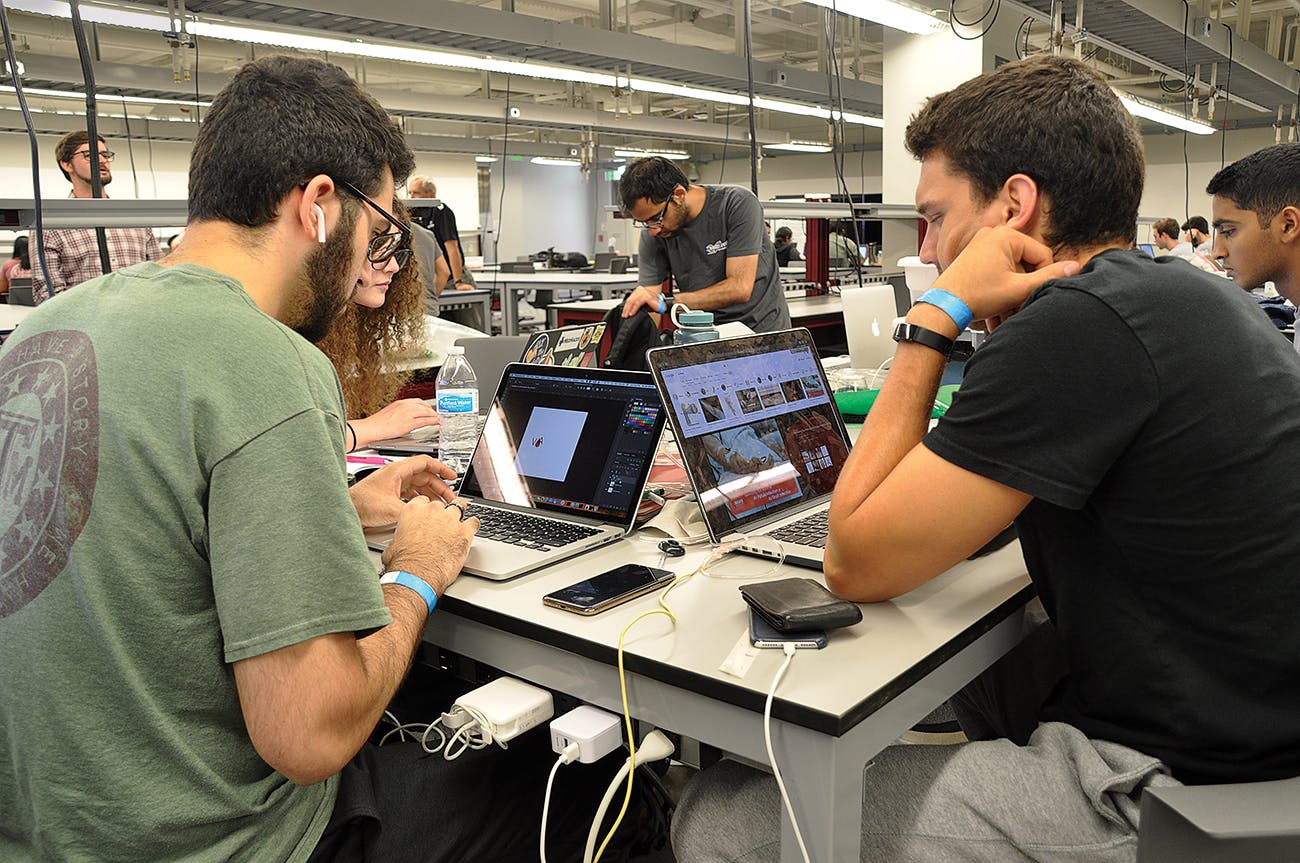
Instruction is largely case-based; professors detail aspects of an imagined patient’s ailment, and students work as teams to improve upon some bit of clinical reasoning they’ve observed. They’re challenged to draw on lessons learned during an engineering class to inform how they would confront each new problem.
For instance, one day they’ll discuss artificial intelligence in an engineering class, and the next day they’ll focus on the typical operations of an emergency room. The question will then be put to them: How might AI be used to more effectively screen patients in order to decide who should be prioritized in a busy ER?
“It’s really nice, because everything we learned, we’re directly applying it,” Gadangi says. “We’re taking our engineering training and putting it at the forefront.”
Just as important to the program as the students’ nitty-gritty engineering knowledge is the engineering mind-set they bring to a problem. Doctors and engineers are taught to solve problems very differently. Where medical students memorize medicine like a foreign language—“That’s almost backward to innovation,” Boone says—engineers are trained to probe the underlying conditions leading to a problem. They want to understand how it might best be solved—not to jump to a conventional solution they’ve learned by rote. “If you attempt to memorize too much in engineering, you will not pass your classes,” says Katherine Banks, A&M’s vice chancellor and dean of engineering and national laboratories. “We want engineering students to move through the design process using mathematics, not just to memorize calculations.”

Both approaches have their uses. If you visit a doctor because of abdominal pain, you’ll be happy that she has memorized the most common causes, knows which tests to run, and can pinpoint what the best treatments are. Chances are you’ll quickly feel better as a result. But what medicine needs more of, says EnMed’s dean, Dr. Roderic Pettigrew, are physicians inclined to take an extra step in their interactions with patients. What tools or tests might be developed to detect earlier the underlying conditions that cause pain? What can be done to avoid having the problem in the first place?
The idea of combining both approaches in a medical school came about nearly four years ago, when Texas A&M Chancellor John Sharp asked Banks to dream up an innovative collaboration between A&M’s engineering department and Houston Methodist. Sharp didn’t have anything specific in mind; his interest lay in enlarging A&M’s presence at the Texas Medical Center, the Houston district that’s home to top research institutions such as the MD Anderson Cancer Center and the Baylor College of Medicine. “There’s just no hundred or two hundred acres anywhere on the globe that’s more important now for health care,” says Sharp, who has been busy raising A&M’s profile since he took over the school nearly a decade ago.
Banks proposed an initiative, EnHealth, that would integrate an engineering mind-set and engineering tools into education and research, beginning with EnMed but eventually reaching A&M’s nursing, dentistry, pharmacy, veterinary, and public health programs.
To lead this effort, Pettigrew, who is also EnHealth’s CEO, was recruited in 2017 from the National Institutes of Health, where he was the founding director of the National Institute of Biomedical Imaging and Bioengineering. Pettigrew, who holds both a PhD in radiation physics and an MD, had seen firsthand the need for greater interaction between medicine and other scientific disciplines when he was a graduate student at the Massachusetts Institute of Technology. There, he’d been working on developing boron neutron capture therapy, which aimed to use microscopic nuclear explosions contained within the diameter of cells to treat brain cancer. The therapy worked on the cancer, but there was a problematic side effect: it also killed blood vessels. “I wanted to be a medical problem solver,” Pettigrew says about his subsequent decision to attend medical school. “I knew I would understand the problems better if I had a firsthand knowledge of medicine.”
After getting his MD, he went on to, among other accomplishments, help pioneer four-dimensional magnetic resonance imaging of the cardiovascular system. Still, Pettigrew wishes he could have earned his degrees simultaneously, in the EnMed fashion. He suspects he would have experienced “a lot more eureka moments because I would have had a more integrated and complete understanding of how life really works.”
With the EnMed method, he says, “you become scientifically bilingual. If you’ve ever known anybody who’s bilingual, they think in both languages. They don’t translate from one to the other. That’s what we want—physicianeers who think in both of these languages.”
There’s no such thing anymore as a lone inventor of truly innovative health-care technology. Medicine has become far too complex for that, says Dr. Paul Yock, the director of Stanford University’s Byers Center for Biodesign. Breakthroughs are possible now only when multidisciplinary teams of bioengineers—specialists in developing medical devices or therapeutic techniques—and physicians work together.
Yock calls the EnMed program a “terrific pilot” for training a new subset of doctors who are capable of leading teams of engineers and physicians and speaking both their languages. “They can talk to the engineers. They can talk to the docs,” he says. “They can help steer a team in a productive direction.”
According to the Association of American Medical Colleges, the accrediting body for most U.S. medical schools, dual-degree programs that allow students to gain expertise in other subjects, such as law and business, are becoming more popular. They’re available to students at all but one accredited medical school in Texas. Yet a 2019 survey by the AAMC found that just 9.3 percent of med school graduates nationwide completed such a program.
And even those who do so are typically taking a year off from their traditional medical training to focus, separately, on earning the second degree. The University of Illinois’s Carle College of Medicine, which welcomed its first class in 2018, is the only medical program in the country other than EnMed that’s teaching medicine with an engineering focus. Carle graduates, however, will receive only medical degrees, not an additional master’s in engineering, as EnMed students will. But perhaps the most significant difference between the programs is A&M’s requirement that its students invent a product or technique in order to graduate.
Banks describes this final project as pivotal to EnMed’s mission. “It brings together everything they’ve learned throughout their entire educational careers to solve a problem,” she says. “That type of capstone—a situation where you are challenged intellectually with a problem and you must come up with a solution—that is red meat for engineers. That is success for us.”
It’s also a manifestation of another of EnHealth’s long-range goals: to turn engineering-inspired ideas into commercially viable solutions. The global medical device market—providing everything from replacement hip sockets to artificial heart valves—is estimated at hundreds of billions of dollars annually and expected to grow significantly in the coming years. EnMed students might well take advantage of such opportunities, though they’re required to cede ownership of any intellectual property they invent while in the program. Instead, they are promised a minority share of any profits from that IP, while the university, hospital, and other partners that may be brought in to facilitate commercialization split the rest.
To encourage such entrepreneurial efforts, the university system is building an engineering design center, where students can access prototyping tools and materials. It’s part of an $85 million renovation of an eighteen-story building A&M purchased about half a mile from Houston Methodist. Beginning this summer it will house much of the EnMed program and, eventually, other components of EnHealth. (A&M plans to construct two more buildings at the Texas Medical Center over the next four years.)
EnMed’s leaders don’t have a clear sense of what their future graduates will do with their degrees. Will they land residencies at top hospitals? Found revolutionary biomedical start-ups? Or maybe develop a new system of telemedicine to serve remote rural communities? The program’s leaders say they’ll be happy to see some students use an engineering mind-set in general practice, where daily interactions with patients might inspire new and more effective treatments.
Innovation in medicine can take many forms and will be spurred, Pettigrew believes, by breaking down the barriers that have been erected between academic disciplines. “Life is a consequence of biology,” he says. “It’s a consequence of physics, of chemistry, of engineering. If you didn’t have all of those, you would not have life.”
This article originally appeared in the February 2020 issue of Texas Monthly with the headline “The Engineer Will See You Now.” Subscribe today.
- More About:
- Health
- John Sharp
- College Station