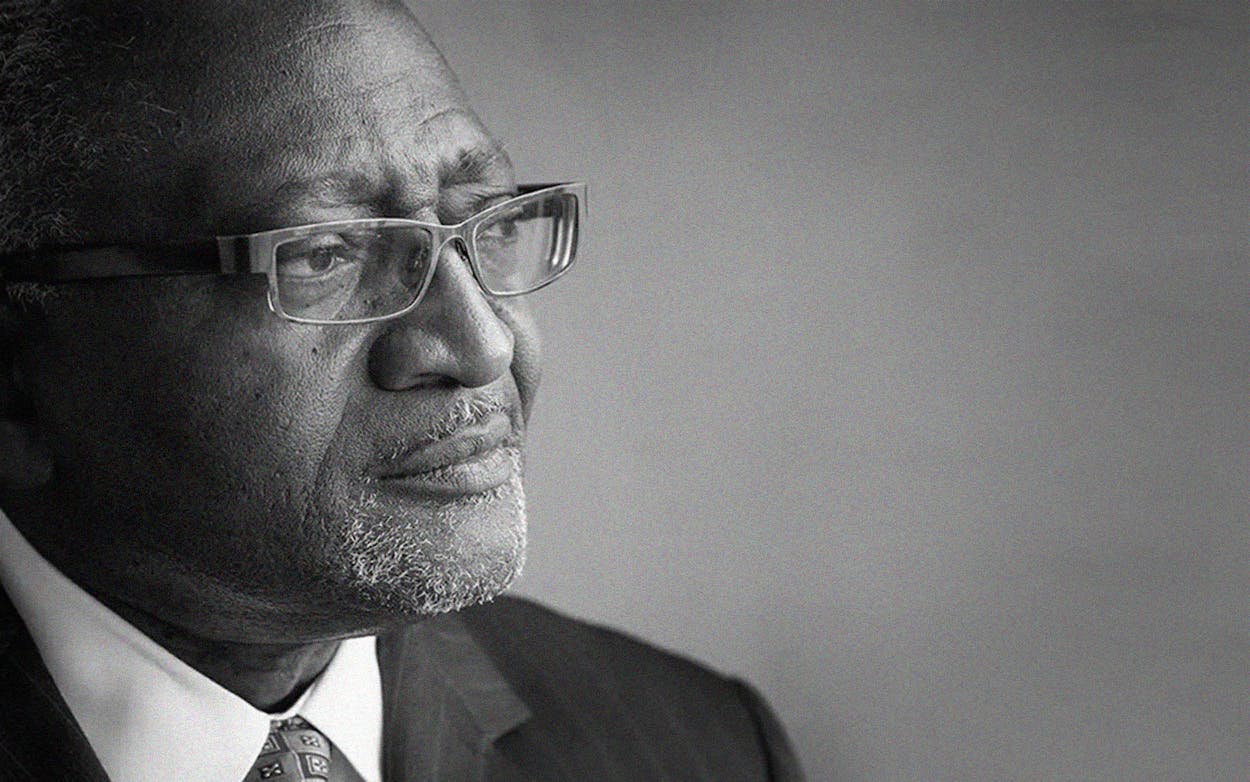
As the coronavirus keeps large swaths of Texas shut down, from the economy to the education system and social life, it has become common to note that the disease “doesn’t discriminate.” But Robert Bullard, a professor and former dean at Texas Southern University’s Barbara Jordan–Mickey Leland School of Public Affairs, has spent the past four decades researching the opposite: how natural disasters and crises wreak havoc on society unequally. Low-income communities of color often have far fewer resources to address disaster and, as a result, face far greater risks than whiter, wealthier neighborhoods in times of crisis.
Indeed, across the nation, evidence suggests that people of color are dying at higher rates from COVID-19 than are white people. Though Texas’s Department of State Health Services has so far reported incomplete racial data, some counties are following the national trend. In Harris County, for example, 40 percent of those who died from COVID-19 were black, though black people account for only 20 percent of the county’s population.
A number of factors could be responsible for the disparity. In Texas, black and Latino communities have higher rates of preexisting conditions that make the coronavirus deadly, like asthma and high blood pressure. When it comes to health care, black, Hispanic, and Native Americans in the state are more likely to be uninsured than white residents, according to data from the Kaiser Family Foundation. Testing for COVID-19 is also far from equally accessible: in the city of Dallas, testing is concentrated in high-income areas. And people of color might also be more likely to be employed in sectors that preclude social distancing: black and Latino workers are the least likely to report being able to work from home, according to the U.S. Bureau of Labor Statistics.
While COVID-19 is a new phenomenon, racial disparities in health outcomes are not. In the seventies, Bullard’s research in Houston demonstrated that toxin-releasing facilities like waste and sewage plants were disproportionately placed in the city’s black neighborhoods, leading to a higher concentration of health problems. To this day, the pattern holds true.
Bullard’s work catalyzed the American environmental justice movement, which argues that environmental problems disproportionately affect communities of color and the poor, and that race and class should be accounted for in their potential solutions. Texas Monthly spoke with Bullard about how the pandemic intersects with environmental issues and why people of color are more vulnerable to the disease.
[This interview has been lightly edited for length and clarity.]
Texas Monthly: In your book The Wrong Complexion for Protection you write, “When societal resources are distributed unequally by class and race, it should be no surprise that population health is distributed along those lines as well.” Were you at all surprised by the racial disparities many counties are reporting with COVID-19?
Robert Bullard: No. When it comes to who gets in line first, and who has priority [for resources like health care], a lot of that is predetermined by the power structures, politically and economic. Oftentimes privilege aligns with race, with white people getting the first and the best protection. And so it’s not surprising when you look at how structural and institutional racism has given privileges for some and disadvantaged others. And when you have poverty, lack of access to health care, [high rates of] uninsured, many who have no private automobiles and are dependent on the buses and public transportation, and neighborhoods in pollution sacrifice zones—and then you pile on top of that the stress of racism—you’re going to get people who are vulnerable. It’s not rocket science. These social determinants of health have been known for many years.
And so the coronavirus is basically taking advantage of those vulnerabilities, and you’re seeing it play out in the deaths. And that’s more than sad. It’s unacceptable.
TM: The coronavirus seems to be a public health disaster that’s layering on top of existing disparities in environmental and social determinants of health. How do you see these things as interconnected, and how are environmental vulnerabilities making the coronavirus worse in certain communities?
RB: We know that if communities are saturated with all kinds of polluting facilities—landfills, incinerators, petrochemical plants and refineries, and coal power plants—and the air quality is bad, you’ll find high rates of ill health: asthma, respiratory illnesses, and other kinds of diseases that are elevated among people of color and poor people, like diabetes and hypertension.
We’re not even dealing with the coronavirus yet: we’re talking about studies that have shown that areas that have high concentration of polluting facilities also have high concentration of health disparities.
So when you apply that to this virus that appears to be attacking the respiratory system … and the cardiovascular system, it’s already hard to breathe in some of these neighborhoods. The coronavirus will make it even harder. It will kill you.
The idea is that if a community is located physically on the wrong side of the levee, the wrong side of the river, on the wrong side of the tracks, it receives less protection than those who are on the right side. Communities of color are disproportionately more vulnerable.
You tell me your zip code, and I can tell you how healthy you are. And so when you talk about trying to map out those social, economic, and racial vulnerabilities, and then overlay health, you can see that there’s a big disparity. You can go from one census tract or one zip code to another, and life expectancy changes by more than fifteen or twenty years by just crossing that line.
TM: Has Texas’s response failed to acknowledge preexisting health disparities?
RB: Texas has the second lowest percentage of testing but that doesn’t surprise me. What surprises me is that it doesn’t have the worst.
This virus does not does not look at your race, or your color. It looks at vulnerability. You can try and look at geographic areas the virus is hitting and not look at race. But then if you put race back in, you will see that there is a discernible pattern. Oftentimes, lax enforcement of environmental law means that communities on the frontline suffer. And that goes hand in hand with lax civil rights enforcement. Texas has the highest rates of uninsurance in the nation, and it has resisted expanding Medicaid, for example. So these policies have created vulnerabilities and it disadvantages communities.
If you talk to people in those neighborhoods on the streets, they can tell you without mapping that they’re most likely to get flooded. Most likely to get polluted. Most likely to suffer from extended unemployment. Or they don’t have the benefit of working from home or a safety net for sick days and paid leave. The medical folks call it comorbidity. Folks on the frontline have always known that’s how things are connected. It’s the cumulative impact of all these things coming at you at one time.
TM: What sort of public policies do you think that Texas, or the United States more generally, should implement to close these racial disparities?
RB: There are some obvious things that need to happen like strengthening people’s access to health care and health insurance. In the last few weeks, we’ve seen attempts to weaken both access to health care and environmental standards with federal rollbacks of specific provisions of the Clean Air Act and tailpipe pollution, and even today with mercury emissions.
So for many of us who have been advocates of environmental justice and health equity, that’s the wrong direction. Other states have taken the high road, and expanded Medicare and access to health insurance. And we should also acknowledge that climate change will make it even more difficult in the future for Texans with hotter days and more bad air-quality days. There will be more outbreaks [because of climate change], as health professionals and scientists have said. We can’t wait to address these issues. We need a real emergency plan for disasters, especially as our population is growing in Texas, to make our cities and rural areas more resilient.
TM: Low income communities are also more likely to live in environmentally vulnerable areas, particularly those at risk of flooding. Do you have concerns about hurricane season coming up and how that might put a double strain on some communities?
RB: The communities that are hit hardest and take the longest to recover, those are the same communities that I’m worried about. On June 1, if we have an active hurricane season in communities that are already suffering from COVID-19, how can you shelter in place when you have to evacuate? Where do people go? If you go to a shelter, it’s going to be hard to social distance. So you’re talking about disasters compounding. That should be worrisome for FEMA and the state government. I’m hoping there is planning for that, so that we don’t get caught flat-footed. I would hope that the smartest people in government are working on the areas that have historically had these severe weather events.
People are stressed about the virus, and people who live on the Gulf Coast, April and May is when they start getting stressed about hurricane season. How are we going to respond to another Harvey or Imelda? In many cases, community groups are the first line of defense. People aren’t going to wait on the government for [immediate aid], because if we do, it will be too late. It’s important to lift up organizations and institutions that have built up that trust in communities. We have to make sure that these organizations are funded and positioned in a way that can address what’s happening.